"All disease begins in the gut"
said Hippocrates, more than 2000 years ago. It may sound exaggerated. That is, if you presented an average physician or scientist with the above claim 20 years ago (actually, for many, it applies even today), they would likely react with a great scepticism. After all, the modern medical science has been able to research all the complicated pathways and molecules in the body, we have seen how complicated it is, it must be far more complex than that! And we are far more advanced than some guy with random thoughts from long ago. Right?
Actually, it turns out that while Hippocrates's idea may be a bit too simplistic, his message pointing to the crucial role of the human gut for our health was very smart and far more advanced than we thought.
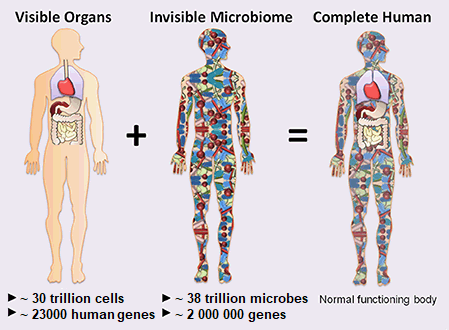
We as humans are not living in this world alone. In each of us, there are trillions of microbes coexisting with us, found mostly in our gut. We call this vast population of microbes the human microbiome.
A new organ, a new medicine
The usual thinking of the past has been of this kind: sure, there are some microbes in the gut, they help us somehow with the digestion, produce certain vitamins, if you get some nasty infection or take antibiotics, something can go wrong with them, but well, okay, nothing too fancy to see there, let's move on.
However, in the recent years it is becoming crystal clear, that there is far, far more to it. The current research is finally showing clearly what many people have been suggesting for a long time.
The human microbiome influences our whole body, our whole functioning, how we feel, sleep, look, what we eat and even what do we think. It goes far beyond just having a good digestion or immunity. By means of producing many substances and also, being connected to complex neural networks of our bodies, the microbiome directly influence our overall health. Studies are already showing that there is in fact a constant interplay, a two-way communication between our gut and our brain, affecting our thinking and mood. In other words, the health of our gut directly influences our mental and emotional state, and vice versa.
The health of our gut directly influences our mental and emotional state, and vice versa.
In the bigger picture, the gut microbiome can be easily thought of as a organ - a very important organ which has not been taken into account until now.
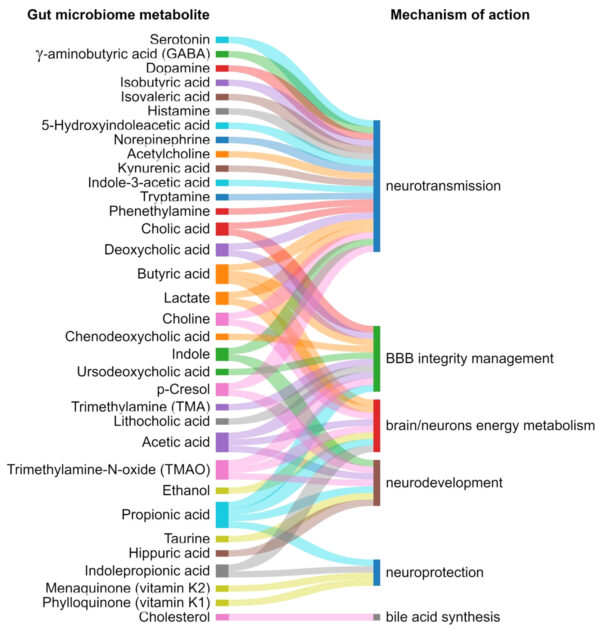 Exemplary gut microbiome metabolites and their mechanism of action in gut–brain communications, mental health and brain development. Source: J.M. Sasso et al.: Gut Microbiome–Brain Alliance: A Landscape View into Mental and Gastrointestinal Health and Disorders, 2023
Exemplary gut microbiome metabolites and their mechanism of action in gut–brain communications, mental health and brain development. Source: J.M. Sasso et al.: Gut Microbiome–Brain Alliance: A Landscape View into Mental and Gastrointestinal Health and Disorders, 2023
We are far more complex than we had ever previously thought.
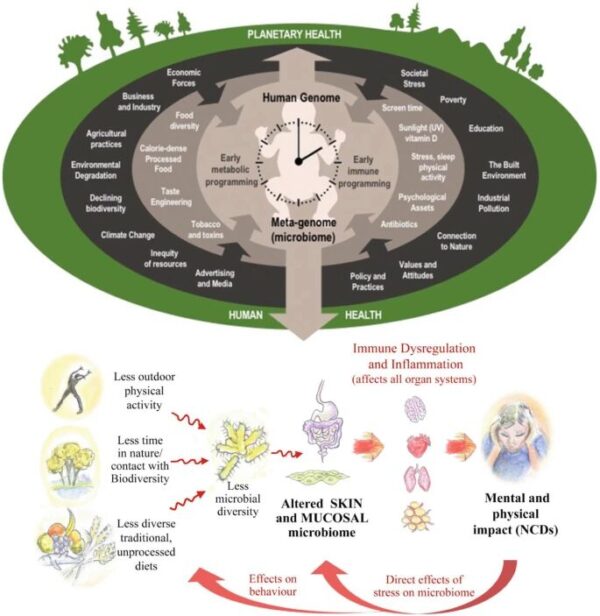
We have evolved side by side with these microbes in us. A disturbance to these little companions (causing so-called "dysbiosis") may result in various health problems. Thus, all aspects of our lives, the medicine as we know it, the drugs we take, the food we eat are showing up in a new, very concerning light. Our modern society with its dubious environment, food and medications are all affecting our microbiomes and disturbing it in ways that had previously not occured for thousands of years.
A healthy microbiome is a must for a good health, both physical and mental. Trying to treat a person paying attention only to superficial manifestations of disease, without taking into account the condition of their gut is at best a questionable, workaround solution, at worst a terrible mistake with potentially tragic consequences.
The inter-relationships between human and ecological health as expressed through the exposome concept (top) and the pathways to reductions in physical health through dysbiosis (bottom). Source: Renz et al. An exposome perspective: early-life events and immune development in a changing world, 2017
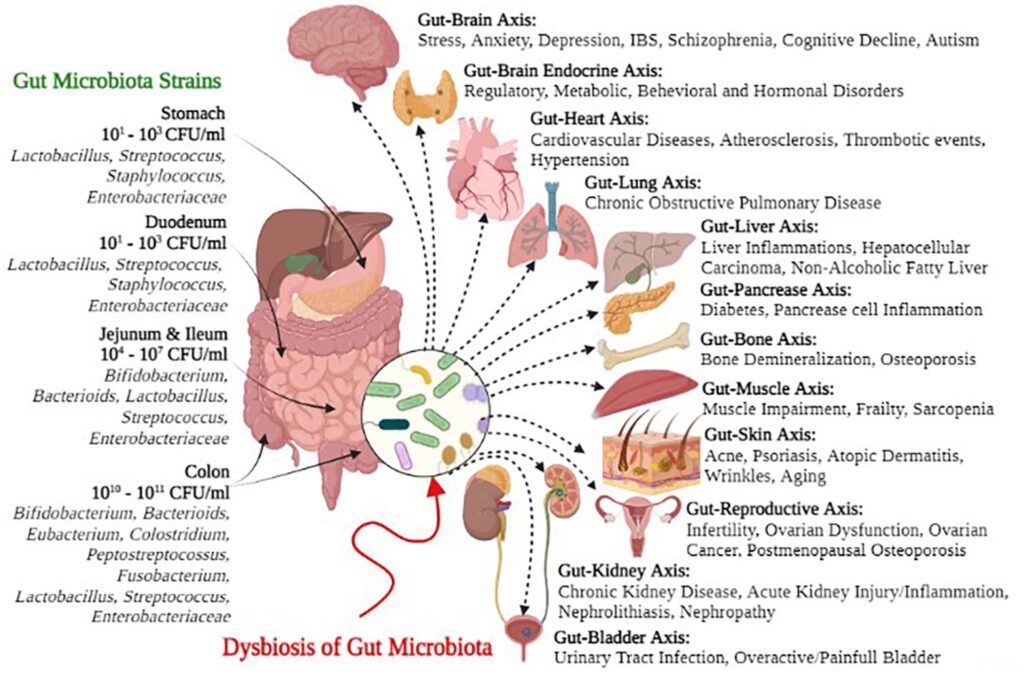
Gut microbial strains and negative health outcomes of gut microbial dysbiosis. Source: M. Afzaal et al.: Human gut microbiota in health and disease: Unveiling the relationship, 2022
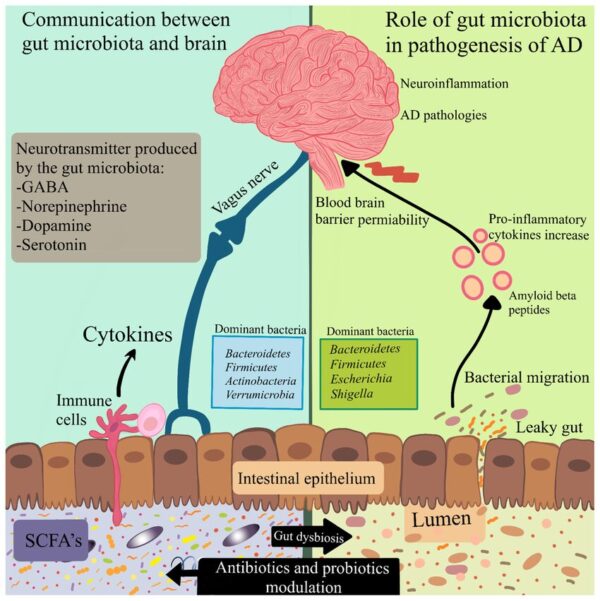
Modulation of the microbiota–gut–brain axis by antibiotics and probiotics. The communication between the gut microbiota and the brain includes neuronal, immune-mediated, and metabolite-mediated pathways. Gut dysbiosis leads to activation of the immune response and alters the production of neurotransmitters as well as bacterial metabolites. These may have a contribution to abnormal signaling through the vagus nerve. Reduction in the integrity of the gastrointestinal barrier causes bacterial migration and inflammation. Pro-inflammatory cytokines induce disruption of the blood–brain barrier permeability. Antibiotics can hinder the growth of certain bacteria, and probiotics have the potential to normalize the gut microbiota in microbiota–gut–brain processes.
Source: A. Megur: The Microbiota–Gut–Brain Axis and Alzheimer’s Disease: Neuroinflammation Is to Blame?, 2020